By ICEERS | April 14 2022
It’s been fifty years since the anti-addictive properties of ibogaine were discovered and finally the dream of those helping people with substance use disorder is coming true – clinical research that will set the stage for policy change and legal access.
In 2020, ICEERS started the first-ever Phase II clinical trial exploring the potential of ibogaine to treat opioid dependency. Conducted at the Sant Joan de Reus Hospital in Spain, the study is testing a novel ibogaine treatment protocol with ascending low doses of ibogaine to support 20 patients to taper off of methadone.
ICEERS is committed to advancing clinical research that supports the development of evidence-informed policy, while collaborating to enable biocultural conservation efforts led by iboga traditionalists in Central Africa based in solidarity, autonomy, land protection, and benefit-sharing.
Context for Studying Opioid Dependency
Over the past few years, several countries have been experiencing an “opioid epidemic” that has been linked, in part, to the misuse of prescription medications. In the United States, opioid overdoses increased by 54% in the largest cities of 16 states, reaching a daily rate of 130 lethal overdoses in the whole country.1 Also in Canada drug overdoses have sky-rocketed.
With the opioid epidemic completely out of control, it is evident that effective treatments for opioid dependency are lacking. The crisis is presenting an opportunity for engaging in clinical research and in policy advocacy to address barriers to conducting research and to providing clinical treatment. Current trends indicate that there is growing interest in the potential of ibogaine for the treatment of substance use disorders and that the demand for evidence to support its use is increasing.
While Spain is not currently experiencing an overdose crisis, following a heroin epidemic in the 1980s, there are many people who remain dependent on methadone. Many have been dependent for 15 years or more, and a number of them are living stable lives (have work, family, housing, etc.) and are experiencing relatively good health.
Over the past few decades, extensive anecdotal evidence from the medical subculture and observational research illustrates that ibogaine is capable of blocking or seriously reducing opioid dependency and alleviating craving from opioids and other drugs for up to several months. However, there has only been one randomized, placebo-controlled clinical trial in which ibogaine was administered to study the pharmacological effects and safety in humans, where researchers provided very small doses of ibogaine (20 mg).2 No other phase 1 clinical trials (in healthy humans) have been conducted as of yet.
The Clinical Trial Protocol
In order to fill in this important research gap, ICEERS has partnered with Sant Joan de Reus University Hospital, in Catalonia (Spain), a hospital recognized for its world-class drug dependency treatment unit. The study is being co-led by Dr. José Carlos Bouso, ICEERS’s scientific director, and Dr. Tre Boras, MD, a psychiatrist and Head of Drug Dependence Services at Sant Joan Hospital. The study is being organized by ICEERS’s Research Coordinator, Genís Oña, MSc, PhD(c).
Through this collaboration, we will conduct a Phase-II Randomized Control Trial with 20 participants, testing a novel ibogaine treatment protocol with ascending low doses of ibogaine to support patients to taper off of methadone.
Methadone is a very long-acting opiate that despite its benefits as an opioid substitution therapy, can result in significant withdrawal symptoms in patients looking to wean from it. Methadone is very difficult to detox from. Therefore, if the protocol we will be employing is successful in supporting participants to detox from methadone using ibogaine, this will provide evidence to support its application with shorter acting opioids, such as heroin.
Based on a previously published case-report,3 we will use a standardized protocol consisting in progressively reducing the methadone dose used, while administering low to mid doses of ibogaine in order to treat opiate withdrawal symptoms. This novel protocol was developed by Clare Wilkins, who also collaborated on elaborating it for use in this trial.
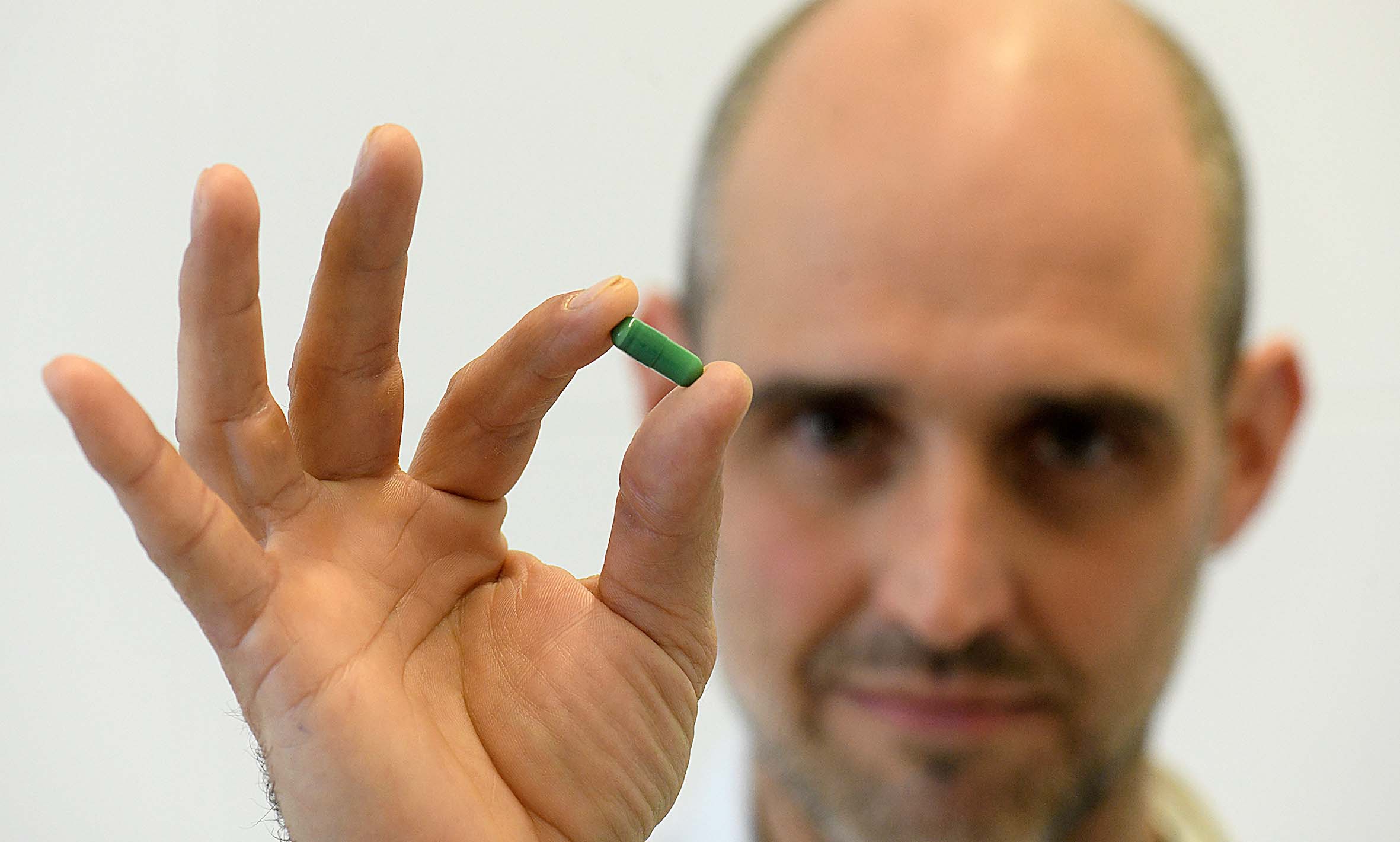
Patients will be split into two randomized groups. Group 1 (n=10) will receive six doses of ibogaine (100 mg each), while Group 2 (n=10) will receive ascending doses of ibogaine, increasing by 100 mg per dose (100-200-300-400-500-600 mg). Ibogaine doses will be administered in a double-blind fashion.
Clinical research findings are essential for creating a pathway for policy change and increasing access to ibogaine as a treatment for substance use dependencies. In Canada, for example, ibogaine has been added to the prescription drug list. However, without clinical trial evidence, it remains unavailable as a prescribed medication.4 It is the hope that this study will be an important contribution to the long-awaited acknowledgement of ibogaine’s medical properties. In an ideal future, the ibogaine produced for use in the West will be ethically sourced and benefits will be shared with the traditional stewards of this sacred medicine in Central Africa.
Thank you to the study’s generous supporters:
- Riverstyx Foundation
- Dr Bronner’s
- Multidisciplinary Association for Psychedelic Studies (MAPS)
- Government of Catalonia
- Nikean Foundation
- Etheridge Foundation
References
- National Institute on Drug Abuse. Opioid Overdose Crisis. [Internet]. United States; 2021. Accessed on 12-3-2022.
- Glue P, Winter H, Garbe K, Jakobi H, Lyudin A, Lenagh‐Glue Z, Hung CT. Influence of CYP2D6 activity on the pharmacokinetics and pharmacodynamics of a single 20 mg dose of ibogaine in healthy volunteers. The Journal of Clinical Pharmacology. 2015 Jun;55(6):680-7.
- Wilkins C, dos Santos RG, Solá J, Aixalá M, Cura P, Moreno E, Alcázar-Córcoles MÁ, Hallak JE, Bouso JC. Detoxification from methadone using low, repeated, and increasing doses of ibogaine: A case report. Journal of Psychedelic Studies. 2017 Mar;1(1):29-34.
- Government of Canada. Notice: Prescription Drug List (PDL): Multiple additions [2017-05-19]. [Internet]. Canada; 2017. Accessed on 12-3-2022.
Categories:
Ibogaine clinical trial
, NEWS
, Iboga and ibogaine
, RESEARCH & INNOVATION
Tags:
ibogaine
, scientific research
, study
, risk reduction
, drug dependence
, withdrawal
, opium