Igor Domsac | October 20, 2025
Psymposium 2025, held between October 2 and 4 this year at the Ilustre Colegio Oficial de Médicos de Madrid, a historic building constructed in 1831, brought together several hundred people—both in person and via livestream—to discuss the present and future of psychedelic-assisted therapies. Organized by the Inawe Foundation, the event brought together clinicians, researchers, and communicators at a key moment, when several European countries have just approved the therapeutic use of substances such as psilocybin and MDMA.
Thursday, October 2
Inawe President Carlos Alonso opened the meeting on Thursday afternoon by reminding attendees that the foundation’s goal is to bring scientific evidence on psychedelics to society and mental health professionals. Vice President Juan Pablo Ramírez then highlighted the need to create safe spaces for dialogue and training in light of growing social and media interest in these therapies.
Pharmacologist and science communicator Antón Gómez-Escolar gave the opening presentation, a visual journey through the history and renaissance of psychedelics from their ritual origins to their current clinical expansion. He showed how scientific publications on psychedelics have skyrocketed in the last decade and reviewed the main regulatory advances in countries such as Germany, the Czech Republic, and Australia. His presentation placed Spain on the cusp of a new era, with hundreds of thousands of people who do not respond to conventional treatments and could benefit from new therapeutic approaches.
The second presentation was given by psychiatrist Óscar Soto Angona, a researcher at Parc Sanitari Sant Joan de Déu and the Autonomous University of Barcelona, who addressed the theoretical basis of psychedelic-assisted psychotherapy. His presentation reviewed the main models that attempt to explain how these substances can facilitate therapeutic change, placing their potential beyond mere pharmacological effects. The psychiatrist presented a theoretical framework for understanding how psychedelics can facilitate processes of profound psychological change. He explained that their action is not limited to the neurochemical level, but rather promotes more plastic and receptive mental states, capable of loosening rigid patterns of thought and emotion.
Soto highlighted the role of extra-pharmacological factors—the so-called set and setting—the relevance of subjective experience, and the therapeutic alliance as essential components of efficacy. From the perspective of dynamic systems theory, he argued that these experiences can temporarily destabilize rigid mental systems to allow for a healthier and more resilient reorganization, always within the framework of appropriate clinical support.
Dr. Irene de Caso offered a rigorous and accessible overview of the neurobiological mechanisms of classic psychedelics—LSD, psilocybin, and DMT—focusing her presentation on how these substances alter perception, cognition, and consciousness. She explained that their action on serotonin 5-HT2A receptors triggers a temporary disorganization of the brain’s functional networks, allowing for a freer flow of information and the dissolution of the usual boundaries of the self. These alterations, which involve the “default neural network” and the medial temporal lobes, can translate into mystical or emotionally transformative experiences.
Irene showed functional resonance images comparing brain activity under placebo and psilocybin, showing an increase in global connectivity and a reduction in hierarchical control of networks. This phenomenon, she explained, is related to the feeling of unity and expansion that many participants describe during the psychedelic experience. She concluded by emphasizing that, far from offering a simple “hallucinogenic trip,” these substances open a privileged window to explore the relationship between the brain, mind, and consciousness.
Finally, researcher Genís Oña, a former member of ICEERS and currently affiliated with the Universitat Rovira i Virgili, presented a historical overview of pioneering work in Spain—from Jordi Camí and Manel Barbanoj to Jordi Riba—and reviewed the most recent doctoral research on substances such as salvinorin, 2C-B, and ibogaine. Oña explained the mechanisms of action on 5-HT2A receptors, showing how their activation reduces the perceptual threshold and increases neuronal excitability, allowing more sensory and emotional information to reach higher levels of processing. He also presented neuroimaging evidence showing greater connectivity between cortical regions under LSD or psilocybin, which is associated with ego dissolution and the emergence of visionary or mystical experiences.
Friday, October 3
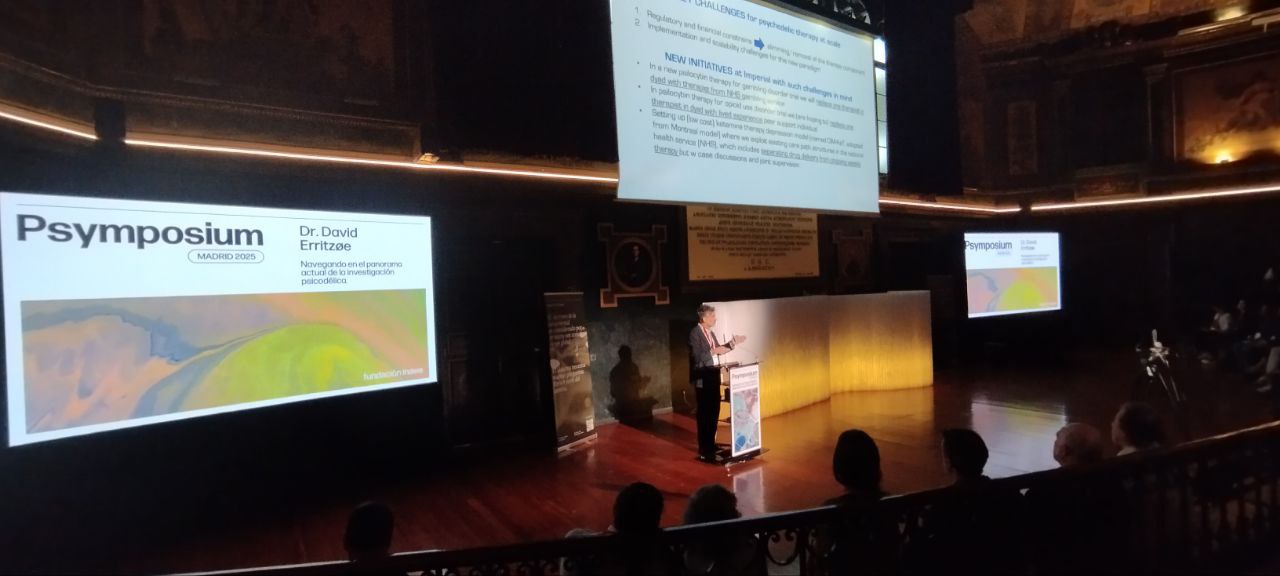
Dr. David Erritzøe, clinical director of the Centre for Psychedelic Research at Imperial College London, opened the second day of the Psymposium with a review of the latest clinical results with psilocybin and DMT in the treatment of depression. His talk presented comparative evidence showing that a single session of psilocybin can generate therapeutic effects equivalent to multiple doses of ketamine, with sustained improvements lasting weeks or months in patients with treatment-resistant depression. Erritzøe emphasized that the key lies not only in the neuroplasticity induced by the substances, but also in the experiential peak, a moment of high emotional and symbolic charge that can catalyze psychological change when properly integrated.
Supported by recent studies from Imperial and other European institutions, the psychiatrist presented neuroimaging data showing greater overall connectivity and less rigidity in brain networks after psilocybin administration, correlated with clinical improvements. He also highlighted the promising progress of trials with controlled-release DMT and psilocybin, noting that these treatments could become viable alternatives for patients who do not respond to conventional antidepressants. He also addressed the main challenges to scaling up psychedelic therapy, such as regulatory limitations, costs, and professional training, and presented new initiatives from Imperial College that seek more accessible models: trials with psilocybin for disorders such as gambling addiction or opioid dependence, and pilot programs in collaboration with the British public health system (NHS) that integrate the experience of peers in therapeutic support.
Psychologist and psychotherapist Marc Aixalà, head of psychological support and integration at ICEERS, gave a presentation focusing on one of the most human—and often least understood—aspects of psychedelic-assisted therapy: integration. He began his presentation by reminding the audience that he does not consider himself a scientist, but rather a clinician who works directly with people, and he emphasized the need to vindicate the psychedelic humanities. Aixalà explained that the only thing all integration models share—regardless of school or context—is the work that follows the experience: reflecting on what has been experienced and applying those lessons to everyday life. From a constructivist perspective, he argued that there is no single reality, but rather multiple ways of interpreting it, and that integration allows the experience to be given meaning within each person’s framework of meaning.
Marc presented a three-phase intervention model—planning, implementation, and integration—that seeks not only to maximize benefits, but also to address the possible complications that may arise after intense or destabilizing experiences. Marc emphasized that the quality of support, prior preparation, and the integration process within a reasonable time frame are decisive factors for therapeutic success.
Dr. Rosa María Dueñas, psychiatrist and researcher at Parc Sanitari Sant Joan de Déu (Barcelona), presented a rigorous overview of the use of psychedelics in the treatment of resistant major depression, which affects about 37% of patients and represents an enormous health and social cost. She compared conventional antidepressants—which are administered daily and have a slow effect—with psychedelics, which show rapid and lasting effects after one or a few doses accompanied by therapeutic support. She highlighted advances with psilocybin, whose clinical trials have shown significant reductions in depressive symptoms and sustained improvements over weeks, along with a restoration of neuroplasticity and brain connectivity.
She also reviewed the evidence on LSD, ketamine/esketamine, and 5-MeO-DMT, noting that these substances share promising potential for addressing resistant cases, albeit with different durations and mechanisms of action. Ketamine, for example, offers rapid relief in acute cases, while psilocybin points to a more transformative and lasting effect. Dueñas emphasized the need for standardized clinical protocols and long-term comparative studies, insisting that safety, support, and integration are essential pillars for transferring these therapies from the laboratory to clinical practice.
Dr. Liliana Galindo, a physician and doctor of neuroscience from the University of Cambridge and member of the Cambridge Psychedelic Research Group, presented a review of psychedelic-assisted therapy in the treatment of post-traumatic stress disorder (PTSD). Based on its high prevalence (around 4% in the general population) and the limited effectiveness of current treatments, she outlined the neurobiological foundations that explain the potential of these therapies: increased neuroplasticity, regulation of the amygdala and default mode network, and facilitation of emotional processing without avoidance.
She explained how empathogens such as MDMA reduce fear and promote openness and interpersonal trust, while classic psychedelics (psilocybin, LSD, ayahuasca, DMT) broaden the emotional range and promote experiences of connection and meaning. In recent studies, MDMA-assisted therapy showed efficacy rates of 50 to 87%, and ketamine between 17 and 67%, with good tolerability and mild adverse effects. Galindo emphasized that the combination of psychotherapy and psychedelic drugs allows traumatic memories to be reconsolidated with less fear, promoting integration and post-traumatic growth, an approach that, she concluded, opens a promising avenue for a comprehensive approach to trauma.
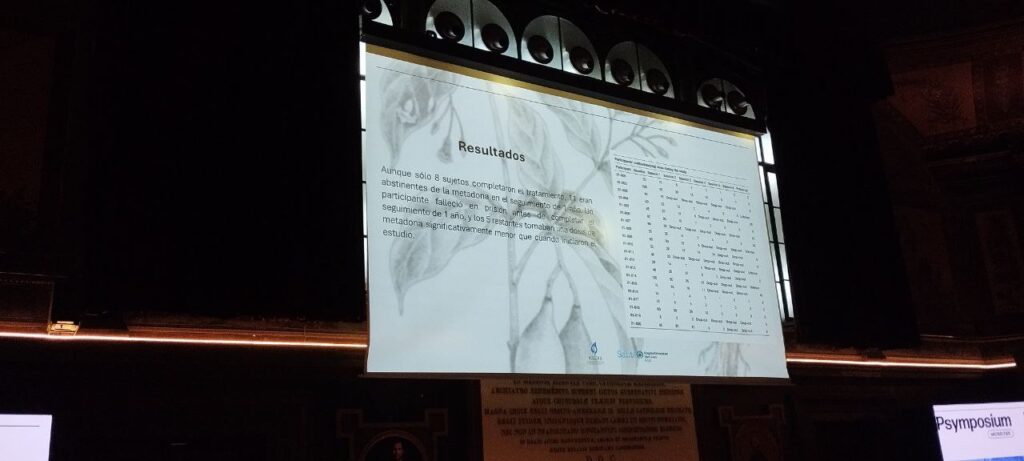
After a coffee break, Dr. Tre Borràs, a psychiatrist and researcher at the Sant Joan de Reus University Hospital, presented the preliminary results of the first clinical trial authorized in Spain with ibogaine, a substance of African origin that is arousing growing interest for its therapeutic potential in the treatment of opioid dependence. The study, conducted in collaboration with ICEERS, evaluates the safety and efficacy of low ascending doses of ibogaine in patients undergoing methadone substitution treatment, with the aim of facilitating a gradual reduction without intense withdrawal symptoms.
Borràs explained that the results are encouraging: after a single dose of 100 to 600 mg, participants were able to significantly reduce their methadone consumption in the following days, with no serious adverse effects reported. VAS assessments revealed transient effects of anxiety and perceptual disturbance, followed by a general feeling of well-being, relaxation, and “reconnection” with oneself. She explained that the findings suggest that ibogaine is safe and effective in reversing methadone tolerance and reducing dependence, without significant cardiac alterations. The psychiatrist also stressed the need for further trials to optimize the dosage regimen and the gradual reduction model. In her conclusions, she emphasized that, beyond sociocultural factors, ibogaine appears to facilitate the relief of withdrawal symptoms, decrease the desire to use, and promote profound change processes, combining neurobiological mechanisms and transformative experiences.
Next, Dr. Sorcha O’Connor presented the initial results of the PsilOCD study, a pioneering investigation into the use of psilocybin in the treatment of obsessive-compulsive disorder (OCD). The trial, which combines clinical and neuroscientific exploration, seeks to evaluate how low and moderate doses of psilocybin can influence cognitive flexibility, neural plasticity (measured by EEG), and the reduction of obsessive-compulsive symptoms.
The study design includes two sessions separated by four weeks—one with 1 mg and the other with 10 mg—in an environment carefully prepared to promote safety and introspection. O’Connor noted that although overall depression scores (MADRS) showed no significant changes, the data suggest that 10 mg of psilocybin may be acting directly on the neurocognitive circuits involved in obsessive behavior, beyond the overall emotional state.
Through testimonials from the participants themselves, the researcher illustrated how some described the experience as a process of self-understanding and distancing from the disorder, with phrases such as “I feel more able to observe my thoughts without identifying with them” or “seeing my problems in a different way makes them easier to deal with.” These accounts point to the therapeutic potential of psilocybin to reconfigure rigid mental patterns, even at moderate doses and without the need for intense experiences.
Subsequently, Dr. Cristina Llagostera, a clinical psychologist specializing in psycho-oncology and palliative care, presented a pilot feasibility study on existential psychotherapy assisted with psilocybin in patients with advanced cancer. Her work explores how this intervention can alleviate the emotional distress and loss of meaning that accompany the end of life.
The protocol includes an experiential session with Psilocybe cubensis extract and three integration sessions (narrative, symbolic, and family). Llagostera highlighted psilocybin’s ability to facilitate acceptance, reduce fear, and restore life purpose in palliative contexts, concluding with the words of Tagore: “Death is not darkness; it is extinguishing your lamp because dawn has come.”
Dr. Débora González, clinical psychologist and professor at Isabel I University, presented the results of a trial on the use of ayahuasca-assisted psychotherapy to address grief after the loss of a loved one. She defined loneliness and emotional disconnection as one of the great contemporary evils and stressed the need to explore tools that facilitate the reconstruction of life meaning.
Based on findings published in Scientific Reports, González showed how ayahuasca can promote acceptance, interpersonal connection, and emotional integration of grief, offering a complementary approach to traditional therapy. Through patient accounts and a review of the Spanish legal framework, she pointed out that attention to existential suffering should be at the center of mental health policies and the development of new psychotherapeutic models.
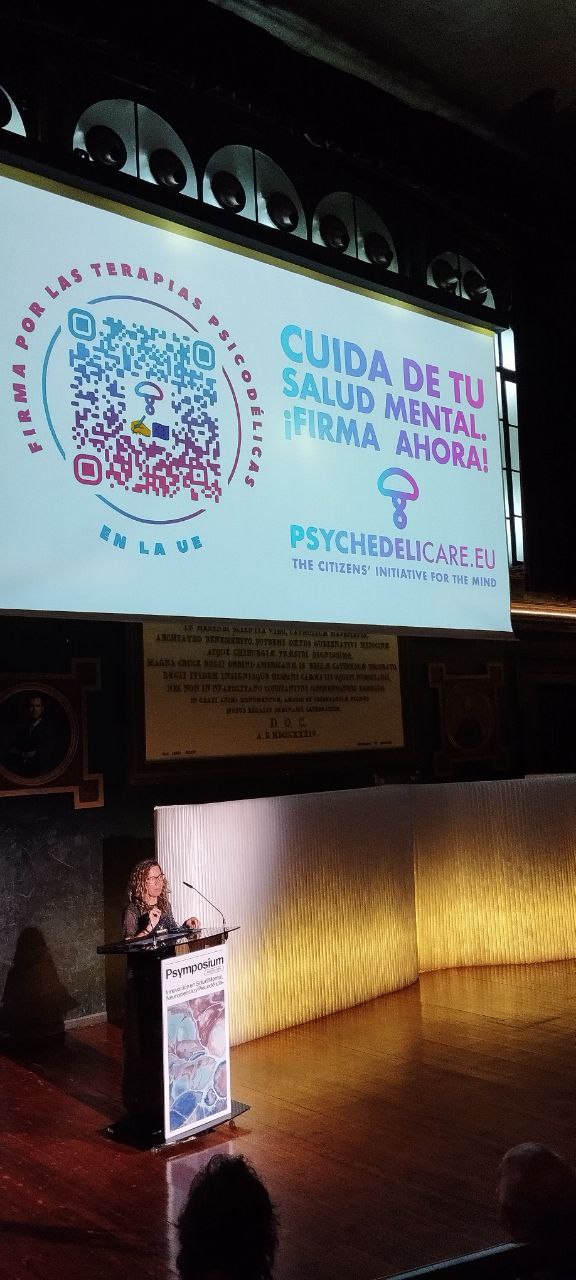
Subsequently, Elisabet Domínguez Clavé, psychologist and doctor of pharmacology, presented the European citizens’ initiative PsychedeliCare, for which she coordinates the team in Spain. This campaign, backed by European entities and organizations such as ICEERS, seeks to collect one million signatures to urge the European Commission to promote regulated access to psychedelic-assisted therapies within mental health systems. Domínguez emphasized that the initiative advocates for an approach based on scientific evidence and the protection of patients’ rights, with the goal of moving Europe toward ethical, safe, and care-centered regulation.
After the lunch break, the day continued with a presentation by Marcela Ot’alora, psychotherapist and trainer for the MDMA-assisted therapy program developed by MAPS, with more than 25 years of experience working with psychedelics. Under the title “The rhythm and nuances of MDMA-assisted therapy: where science and storytelling go hand in hand,” she shared her thoughts on the role of the therapist in the process of accompanying people with post-traumatic stress disorder (PTSD).
Throughout her presentation, Ot’alora addressed essential aspects such as empathic presence, trust, and care in the therapeutic relationship, as well as the importance of respecting the internal pace of each patient’s process. Her presentation combined clinical and human elements, showing how therapeutic practice draws on both scientific evidence and the relational experience that emerges during sessions.
The afternoon continued with the round table discussion “Therapeutic horizons and frontiers: risks and benefits in clinical use,” moderated by Marta Pérez Carmona and with the participation of Dr. Liliana Galindo, Dr. Rosa Dueñas, Dr. Manuel Ángel Franco, and Dr. Óscar Álvarez Bobo. The dialogue revolved around the limits, possibilities, and ethical dilemmas raised by the clinical application of psychedelics.
Among the most debated topics was a question of focus: are we talking about psychedelic-assisted therapy or therapy-assisted psychedelics? A subtle but significant difference that points to the centrality—depending on your point of view—of the therapeutic process or the substance. The speakers agreed on the need to integrate scientific evidence with human experience and ethical support in this new field of mental health.
After the coffee break, the Psymposium closed its first day with one of the most moving panels: “The other perspective: the patient’s point of view,” moderated by Juan París. Andrea Siclari, Elisa Argilés, Luis Barboza, and María Concepción Moldón (Conchi) participated in the panel, sharing their personal experiences in clinical trials with psilocybin and 5-MeO-DMT.
Conchi, a native of Zamora and participant in the Compass Pathways trial with psilocybin for resistant depression, recounted with great emotion her process of transformation after years of suffering and disconnection. She thanked the medical team that accompanied her—especially Dr. Manuel Ángel Franco and his therapists—and described her experience with psilocybin as “a miracle,” a turning point that restored her vitality and desire to live. Her words, filled with gratitude and hope, drew a standing ovation from the audience.
Andrea Siclari, a Swiss participant in the LSD clinical trial for cancer patients conducted in Switzerland, offered a deeply serene account of his transformation process after being diagnosed in 2019 with advanced cancer with metastases. Married with three young children, he described how the disease abruptly halted his life and plunged him into intense anxiety about the proximity of death. “Suddenly, everything stopped,” he said, recalling the operations, aggressive chemotherapy, and months of isolation during the pandemic. In his search for meaning and relief, he decided to participate in the clinical study, which combined psychotherapy with LSD sessions in a controlled environment.
During the first experience, he underwent a process of dissolution of the self and communion with the whole: “The boundaries between myself and my surroundings disappeared… I understood that my life here is only an infinitely small part of who I am.” That transformative experience allowed him to free himself from the fear of dying and reconcile himself with life. “Since then, every emotion has its place: there are no longer negative or positive emotions, they simply are,” he said. In a reflective tone, he explained how the treatment not only reduced his existential anxiety, but also helped him to become more flexible in his role as a father, professional, and friend: “Now I am more myself.”
Dr. Luis Barboza, a primary care physician and participant in a clinical trial with 5-MeO-DMT conducted by the Beckley Foundation, shared his experience from a dual perspective: that of a healthcare professional and that of a patient. He recounted how he came to the study after years of resistant depression and growing exhaustion at the lack of results from conventional treatments. “The whole process was very difficult,” he acknowledged, explaining that even the latest antidepressants caused adverse effects that affected his memory and ability to communicate.
During the experimental session, he described an intense and immediate experience, characterized by a feeling of death and dissolution of the ego, in which he saw himself “outside the body, going through a tunnel.” Although he initially felt fear, he later understood that this transition symbolized the possibility of rebirth. His account illustrated with great humanity the transformative potential of psychedelic therapies when applied in safe clinical settings with appropriate professional support.

Elisa Argilés, a financial sector worker, gave one of the most powerful testimonies at the round table. After more than twenty years living with depression resistant to conventional treatments, she recounted how her life had been reduced to hopelessness, insomnia, and a constant desire not to wake up the next day. Antidepressants stopped working, and her doctor even told her that she had to accept that she would be “a depressed person forever.” That moment, she recalled, led her to seek alternatives and finally to enter the BPL003 clinical trial with 5-MeO-DMT at the Parc Sanitari Sant Joan de Déu in Barcelona.
The experience marked a turning point. Elisa emphasized the importance of preparation and therapeutic integration, which allowed her to overcome her fear and break the mental patterns she had held for decades. “I was cured in the moment,” she said, “but the real work began afterwards, every day, choosing not to repeat the past.” Since then, her mood and her way of relating to life have changed completely: “I came out of the trial with a vitality I hadn’t felt in over twenty years.” Her sincere and hopeful testimony summed up the human potential behind psychedelic research.
Saturday, October 4
Saturday began with a keynote speech by Dr. Tomáš Páleníček, a neuroscientist and psychopharmacologist at the National Institute of Mental Health in the Czech Republic and one of the most renowned researchers in the field of psychedelic neuroscience. In his presentation, entitled “New Advances in Psychedelic Research,” he presented his team’s latest progress in studying the neurobiological and behavioral mechanisms associated with the use of substances such as psilocybin, LSD, and ketamine, with a special focus on the role of brain connectivity and synaptic plasticity. His presentation offered a rigorous and up-to-date overview of the state of preclinical and clinical research in Central Europe, marking the start of a high-level scientific conference.
The round table discussion “Legislation and Implementation of Psychedelic-Assisted Therapy,” moderated by Dr. Luis Caballero, brought together Dr. Tomáš Páleníček, Dr. Andrea Jungaberle, Antón Gómez-Escolar, and Jerónimo Mazarrasa, program director at ICEERS, to analyze the different regulatory frameworks that are emerging around the world. Jungaberle presented the case of Germany, where the recent approval of compassionate use of psilocybin sets a precedent in Central Europe. Gómez-Escolar reviewed experiences outside the continent—such as Canada, Australia, and the United States—highlighting the differences between models of medical access, state regulations, and citizen initiatives. Páleníček explained the situation in the Czech Republic, where compassionate use is permitted but commercialization remains restricted, while Mazarrasa offered a critical reflection on the global shift in policies: from a Europe that was a pioneer to a landscape where America leads with more open and experimental approaches.
The keynote lecture by Dr. Magí Farré, professor of Pharmacology and head of department at Germans Trias i Pujol University Hospital, offered a comprehensive review of the clinical pharmacology of MDMA. Farré explained in detail the mechanisms of action of this substance, derived from phenethylamine, and its effect on serotonin, dopamine, and norepinephrine transporters. Using experimental data, he described how MDMA increases the release of neurotransmitters and generates empathic and prosocial effects, which supports its therapeutic potential in the treatment of post-traumatic stress disorder (PTSD).
The speaker also discussed international clinical trials seeking FDA approval for the medical use of MDMA, and compassionate use programs in countries such as Australia, Switzerland, and Canada. His technically rigorous presentation provided an understanding of the scientific basis for MDMA-assisted therapy and the importance of its application in controlled clinical settings.
The lecture by Dr. Chris Timmermann, a researcher at Imperial College London’s Centre for Psychedelic Research, was one of the most eagerly awaited at the Psymposium. Under the title “Psychedelics for the deconstruction of consciousness and the reconstruction of meaning,” Timmermann explored the results of his studies with DMT and 5-MeO-DMT, delving into how these substances can produce experiences of ego dissolution and states of consciousness comparable to those achieved by advanced meditators.
Drawing on recent neuroscientific data, he explained how psychedelics increase brain entropy—a measure of the “chaos” or flexibility of the nervous system—and how this temporary destructuring can open the door to processes of personal meaning reconstruction. Timmermann emphasized the central importance of subjective experience for therapeutic efficacy and highlighted the role of the therapist as an empathetic guide in the integration of meaning. His presentation included a poetic reference to the “fertile void,” that dimension where the loss of references becomes a source of understanding and existential renewal.
Dr. José Carlos Bouso, scientific director of ICEERS, gave an overview of fifteen years of clinical and community research with psychoactive plants. He began with pharmacokinetic studies (e.g., differences in detection between smoked and oral routes and their metabolism) and “natural laboratories” in Brazil, where they compared regular ayahuasca users and controls: far from the hypothesis of neurotoxicity, they found better memory performance, orderly lives, and stable personalities, results that were replicated the following year. Back in Spain, using computerized tests and magnetic resonance imaging, they observed structural changes in brain regions and, in an expanded cohort (ayahuasca users, cannabis users, and controls), no neuropsychological differences but differences in personality traits, which led them to question whether long-term effects should be measured only with cognitive tests. With pre-post designs in ceremonies, around 80% improved their mood, and Bouso stressed the importance of reporting adverse effects: around 25-30% reported some event (including complex cases), although many participants integrated them as part of their process.
The second block addressed traditional contexts and public health: studies at a center in Peru with traditional healers showed sustained improvements by diagnosis; introduced the framework of “symmetrical global mental health” and the “medical systems” approach (not just molecules), with projects such as Maja Kohek‘s in Catalonia and a program with ASOMASHK to describe the indigenous medical system as it functions in the community (where, he noted, patients often do not ingest the plant but receive ícaros). He presented analyses of more than 15,000 cases of adverse effects (≈55% reported some psychological effect; ≈80% considered them part of their transformation) and health surveys suggesting a self-care bias: better indicators not “because of” ayahuasca, but because those who use it are already seeking well-being. During the pandemic, his questionnaires showed that moderate use of psychedelics correlated with better coping strategies. She closed with two ongoing lines of research: a specific scale for experiences with ibogaine and a theoretical model for integrating MDMA into restorative justice and conflict transformation (with Constanza Sánchez Avilés and Jorge Ollero), announced for presentation at Nexus 2025 and future dissemination on the MAPS website.
Dr. Inés Erkizia, pharmacist and researcher at the University of the Basque Country (UPV/EHU), presented the lecture “Preclinical advances in psilocybin research: psychedelic mechanism and antidepressant effect.” Her presentation addressed the gap between the extensive clinical evidence available and the scarcity of preclinical studies that would allow us to understand the neurobiological mechanisms behind the therapeutic effects of psilocybin. She showed experiments conducted with animal models, in which she evaluated the head-tossing response (HTR)—an indicator of the serotonergic effect mediated by the 5-HT2A receptor—and explained how treatment with psilocybin managed to reverse depressive behaviors in models of chronic stress. Erkizia emphasized that the psychedelic effects are mediated by endogenous cortical serotonergic neurotransmission, a phenomenon that could have important clinical implications.
In her conclusions, he pointed out that psilocin (the active metabolite of psilocybin) has a comparable pharmacodynamic profile in humans and rodents, and that the specific antidepressant mechanism of the substance remains largely unknown, especially the role of the acute psychedelic experience in its therapeutic efficacy. Among future lines of research, she pointed to the need to explore the interaction between classic antidepressants and psilocybin, the effects of antidepressant withdrawal on its results, and the neurochemical changes induced in key brain regions such as the prefrontal cortex and hippocampus.
The round table discussion “Psychedelic Research in Spain,” moderated by Dr. Gustavo Díez, rbrought together leading figures from various academic and clinical fields—Dr. Magí Farré, Dr. José Carlos Bouso, Dr. Débora González, and Dr. Óscar Soto Angona—to outline the current state of the field and the challenges it faces in the country. The dialogue addressed everything from scientific advances and the diversity of research models to the regulatory and ethical limitations that hinder the development of clinical trials with psychedelic substances. The speakers agreed on the need to strengthen interdisciplinary collaboration and promote a regulatory framework that allows for rigorous and safe research, placing Spain in the international conversation on psychedelic-assisted therapies.

The final panel of the Psymposium, “Designing the future of the therapeutic use of psychedelics,” brought together Tre Borràs, Marcela Ot’Alora, José Carlos Bouso, and Rosa María Dueñas, moderated by Dr. Luis Caballero, to reflect on the challenges that will mark the next stage of this scientific and clinical revolution. They discussed the ethical integration of these therapies, the training of qualified professionals, the regulation of access, and the importance of not losing sight of the human and relational dimension of the therapeutic process.
After an intense exchange of perspectives, Luis Caballero offered a summary and closing remarks that underscored the need for constant dialogue between science, clinical practice, and society. The closing ceremony, led by Carlos Alonso, president of the Inawe Foundation, served to thank the speakers and attendees for their participation and reaffirm the organization’s commitment to research, education, and responsible development in the field of psychedelics in Spain and beyond.
Psymposium Madrid 2025 marked a real turning point in the debate on the present and future of psychedelic research in Spain. Over three days, scientists, healthcare professionals, and patients shared evidence, experiences, and perspectives that reflect the maturity and diversity of this expanding field. Beyond the results and presentations, the meeting left one clear conclusion: the urgency of building a model of therapeutic innovation based on evidence and guided by care, ethics, and social responsibility, where science and humanity advance together in the exploration of new ways of addressing mental health.
Categories:
Noticias
, NEWS
Tags:
Madrid
, therapeutic innovation
, neuroplasticity
, treatment-resistant depression
, trauma
, Psymposium
, neuroplasticidad
, innovación terapéutica
, INAWE
, depresión resistente
, congreso
, neuroscience
, neurociencia
, ibogaine
, ICEERS
, research
, psychedelic-assisted therapy
, psychotherapy
, mental health
, conference
, psychedelics
, psilocybin
, MDMA
, scientific research
, science

